Search
- Page Path
- HOME > Search
- Clinical Study
- Comparison of the Efficacy and Safety of Insulin Detemir Administered Once Daily According to Two Titration Algorithms (3-0-3 and 2-4-6-8) in Patients with Type 2 Diabetes Mellitus
- Hea Min Yu, Kang Seo Park, Jun Hwa Hong, Keun Yong Park, Jong Min Lee, Bon Jeong Ku, Yeo Joo Kim, Tae Kun Oh
- Endocrinol Metab. 2020;35(1):142-148. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.142
- 4,746 View
- 80 Download
- 3 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
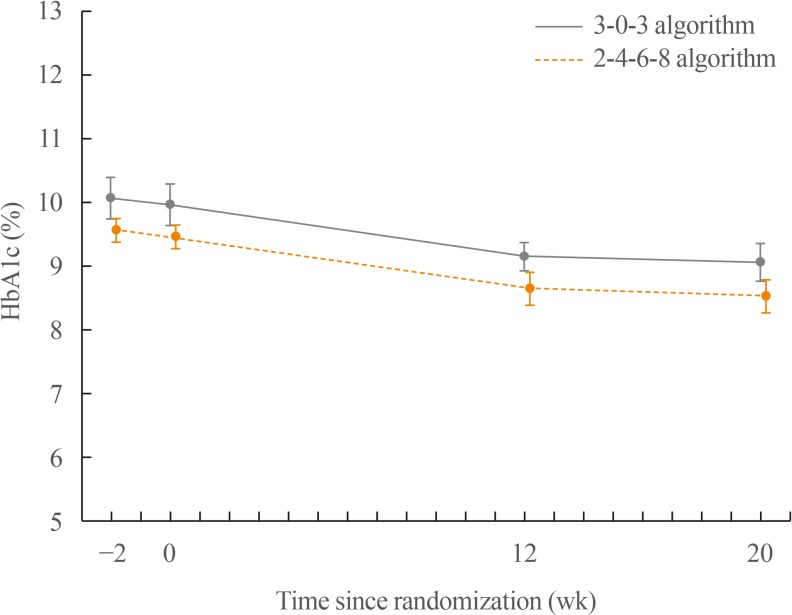
ePub Background This study was conducted to compare glycaemic control with insulin detemir administered according to two titration algorithms (3-0-3 and 2-4-6-8) after 20 weeks of treatment in subjects with type 2 diabetes mellitus inadequately controlled on metformin.
Methods This was a 20-week, randomised, multicentre, open-labelled, treat-to-target trial. Forty-six patients were randomised in a 1:1 manner to either the 3-0-3 (G3,
n =23) or 2-4-6-8 (G2,n =23) algorithm. The primary endpoint was change of haemoglobin A1c (HbA1c), and the secondary safety endpoint included hypoglycaemic events.Results After 20 weeks, HbA1c decreased similarly in the G3 and G2 groups, with a mean change of −0.9% from baseline. The mean change in fasting plasma glucose was numerically similar in both groups. The hypoglycaemia event rate per 100-patient-years of exposure (
r ) in the G2 group (r =1,427) was higher than that in the G3 group (r =807).Conclusion Both treatment groups had numerically similar HbA1c reductions. A trend towards fewer hypoglycaemia episodes after dose stabilisation was seen with the simpler G3. Clinically, this may be an important observation, as a simpler titration algorithm may support self-management and maintenance of insulin therapy.
-
Citations
Citations to this article as recorded by- Time for Using Machine Learning for Dose Guidance in Titration of People With Type 2 Diabetes? A Systematic Review of Basal Insulin Dose Guidance
Camilla Heisel Nyholm Thomsen, Stine Hangaard, Thomas Kronborg, Peter Vestergaard, Ole Hejlesen, Morten Hasselstrøm Jensen
Journal of Diabetes Science and Technology.2022; : 193229682211459. CrossRef - Efficacy and safety of patient-led versus physician-led titration of basal insulin in patients with uncontrolled type 2 diabetes: a meta-analysis of randomized controlled trials
Marco Castellana, Filippo Procino, Rodolfo Sardone, Pierpaolo Trimboli, Gianluigi Giannelli
BMJ Open Diabetes Research & Care.2020; 8(1): e001477. CrossRef
- Time for Using Machine Learning for Dose Guidance in Titration of People With Type 2 Diabetes? A Systematic Review of Basal Insulin Dose Guidance

- Thyroid
- Papillary Thyroid Carcinoma: Four Cases Required Caution during Long-Term Follow-Up
- Hea Min Yu, Jae Min Lee, Kang Seo Park, Tae Sun Park, Heung Young Jin
- Endocrinol Metab. 2013;28(4):335-340. Published online December 12, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.4.335
- 3,800 View
- 28 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Due to the increased prevalence of papillary thyroid carcinoma (PTC), difficult cases and unexpected events have become more common during long-term follow-up. Herein we reported four cases that exhibited poor progress during long-term follow-up. All the cases were diagnosed with PTC and treated with total thyroidectomy before several years, and the patients had been newly diagnosed with recurrent and metastatic PTC. These four cases included recurred PTC with invasion of large blood vessels, a concomitant second malignancy, malignant transformation, and refractoriness to treatment. Physicians should closely monitor patients to promptly address unforeseen circumstances during PTC follow-up, including PTC recurrence and metastasis. Furthermore, we suggest that the development of a management protocol for refractory or terminal PTC is also warranted.
-
Citations
Citations to this article as recorded by- Induction of epithelial-mesenchymal transition in thyroid follicular cells is associated with cell adhesion alterations and low-dose hyper-radiosensitivity
Ankit Mathur, Vijayakumar Chinnadurai, Param Jit Singh Bhalla, Sudhir Chandna
Tumor Biology.2023; 45(1): 95. CrossRef - Thyroglobulin Level in Fine-Needle Aspirates for Preoperative Diagnosis of Cervical Lymph Node Metastasis in Patients with Papillary Thyroid Carcinoma: Two Different Cutoff Values According to Serum Thyroglobulin Level
Min Ji Jeon, Won Gu Kim, Eun Kyung Jang, Yun Mi Choi, Yu-Mi Lee, Tae-Yon Sung, Jong Ho Yoon, Ki-Wook Chung, Suck Joon Hong, Jung Hwan Baek, Jeong Hyun Lee, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Thyroid.2015; 25(4): 410. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Induction of epithelial-mesenchymal transition in thyroid follicular cells is associated with cell adhesion alterations and low-dose hyper-radiosensitivity

- Thyroid
- Graves' Disease that Developed Shortly after Surgery for Thyroid Cancer
- Hea Min Yu, Soon Hyun Park, Jae Min Lee, Kang Seo Park
- Endocrinol Metab. 2013;28(3):226-230. Published online September 13, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.3.226
- 3,164 View
- 31 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Graves' disease is an autoimmune disorder that may present with various clinical manifestations of hyperthyroidism. Patients with Graves' disease have a greater number of thyroid nodules and a higher incidence of thyroid cancer compared with patients with normal thyroid activity. However, cases in which patients are diagnosed with recurrence of Graves' disease shortly after partial thyroidectomy for thyroid cancer are very rare. Here we report a case of hyperthyroid Graves' disease that occurred after partial thyroidectomy for papillary thyroid cancer. In this case, the patient developed hyperthyroidism 9 months after right hemithyroidectomy, and antithyroglobulin autoantibody and thyroid stimulating hormone receptor stimulating autoantibody were positive. Therefore, we diagnosed Graves' disease on the basis of the laboratory test results and thyroid ultrasonography findings. The patient was treated with and maintained on antithyroid drugs. The mechanism of the recurrence of Graves' disease in this patient is still unclear. The mechanism may have been the improper response of the immune system after partial thyroidectomy. To precisely determine the mechanisms in Graves' disease after partial thyroidectomy, further studies based on a greater number of cases are needed.
-
Citations
Citations to this article as recorded by- Graves’ disease diagnosed in remnant thyroid after lobectomy for thyroid cancer
Meihua Jin, Ahreum Jang, Won Gu Kim, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Min Ji Jeon, Byeong-Cheol Ahn
PLOS ONE.2022; 17(3): e0265332. CrossRef - Graves’ thyrotoxicosis soon after hemithyroidectomy for low-risk papillary thyroid carcinoma
Ahmad Housin, Michael Tamilia
BMJ Case Reports.2022; 15(5): e250149. CrossRef - Effects of energy-based ablation on thyroid function in treating benign thyroid nodules: a systematic review and meta-analysis
Yuan Fei, Yuxuan Qiu, Dong Huang, Zhichao Xing, Zhe Li, Anping Su, Jingqiang Zhu
International Journal of Hyperthermia.2020; 37(1): 1090. CrossRef - Total Thyroidectomy for Thyroid Cancer Followed by Thyroid Storm due to Thyrotropin Receptor Antibody Stimulation of Metastatic Thyroid Tissue
Lars Folkestad, Frans Brandt, Thomas Brix, Marianne Vogsen, Lars Bastholt, Peter Grupe, Jeanette Krogh Petersen, Laszlo Hegedüs
European Thyroid Journal.2017; 6(5): 276. CrossRef - Percutaneous microwave ablation of thyroid nodules: effects on thyroid function and antibodies
Kristina Heck, Christian Happel, Frank Grünwald, Huedayi Korkusuz
International Journal of Hyperthermia.2015; 31(5): 560. CrossRef - Development of Thyroid-Associated Ophthalmopathy in Patients Who Underwent Total Thyroidectomy
Sun Young Jang, Ka Hyun Lee, Jong Rok Oh, Bo Yeon Kim, Jin Sook Yoon
Yonsei Medical Journal.2015; 56(5): 1389. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Graves’ disease diagnosed in remnant thyroid after lobectomy for thyroid cancer

- A Case of Simultaneous Presentation of Thyroid Crisis and Diabetic Ketoacidosis.
- Kyung Ae Lee, Kyung Taek Park, Hea Min Yu, Heung Yong Jin, Ji Hyun Park, Hong Sun Baek, Tae Sun Park
- Endocrinol Metab. 2012;27(1):63-67. Published online March 1, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.1.63
- 2,097 View
- 31 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Two important endocrine emergencies, thyroid crisis and diabetic ketoacidosis (DKA), are uncommon when presented together, but pose serious complications. Without appropriate management, they may result in high mortality. Although several cases of simultaneous presentation of thyroid crisis and DKA have been reported, it is a clinically unusual situation and remains a diagnostic and management challenge in clinical practice. We report rare case with simultaneous presentation of thyroid crisis and DKA without previous warning symptoms. A 23-year-old-woman was brought to the emergency department presenting with acute abdominal pain for one day. She was healthy and there was no personal history of diabetes or thyroid disease. Through careful physical examination and laboratory tests, the patient was diagnosed with thyroid crisis combined with DKA. Concomitance of these two endocrine emergencies led to sudden cardiac arrest, but she was successfully resuscitated. This emphasizes the importance of early recognition and prompt management when the two diseases are presented concomitantly.
-
Citations
Citations to this article as recorded by- Health Behaviors and Risk Factors Associated with Chronic Kidney Disease in Korean Patients with Diabetes: The Fourth Korean National Health and Nutritional Examination Survey
Suk Jeong Lee, Chae Weon Chung
Asian Nursing Research.2014; 8(1): 8. CrossRef
- Health Behaviors and Risk Factors Associated with Chronic Kidney Disease in Korean Patients with Diabetes: The Fourth Korean National Health and Nutritional Examination Survey


 KES
KES

 First
First Prev
Prev



